Factors influencing treatment selection and thirty-day mortality following chemotherapy for people with small cell lung cancer: an analysis of national audit dataTools Jones, Gavin S., McKeever, Tricia M., Hubbard, Richard B., Khakwani, Aamir and Baldwin, David R. (2018) Factors influencing treatment selection and thirty-day mortality following chemotherapy for people with small cell lung cancer: an analysis of national audit data. European Journal of Cancer . ISSN 0959-8049 (In Press)
AbstractBackground
Actions (Archive Staff Only)
|

 Tools
Tools Tools
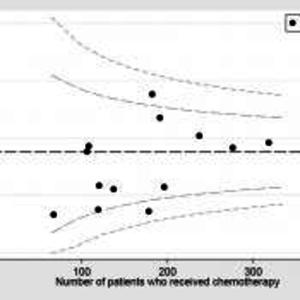
Tools![Figure 1 [thumbnail of Figure 1]](https://eprints.nottingham.ac.uk/54974/2.hassmallThumbnailVersion/file.jx1.jpg)
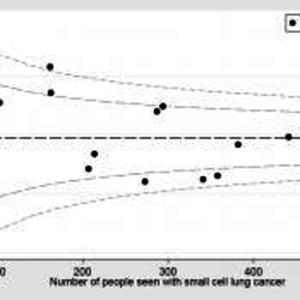
![Figure 2 [thumbnail of Figure 2]](https://eprints.nottingham.ac.uk/54974/3.hassmallThumbnailVersion/file.jx.jpg)